Innovation that remains ahead of its time.
Even after 20 years, unmatched clinical evidence has helped Apligraf® remain the biotech healer capable of transforming wounds from chronic to acute and heal VLUs and DFUs faster.1-8
See how Apligraf transforms
wounds from chronic to acute
Take a closer look at how the mechanism of action of Apligraf helps to heal VLUs and DFUs faster.1-8
To skip to a different chapter of the video, click on a dot in the progress bar. The chapters are: (1) What Is Apligraf? (2) The Power of Living Cellular Technology. (3) Overcoming Barriers to Healing. (4) Clinical Evidence and Coverage. (5) Why Apligraf?
Designed to heal even in the most
challenging environments
Apligraf is a skin substitute that looks, functions, and responds like healthy skin.2,9-11

layer Dermal
layer
Epidermal layer: Contains living keratinocytes and stem cells that provide potent healing signals (growth factors/cytokines)2,10,11
Dermal layer: Contains living fibroblasts that proliferate and produce human collagen and other ECM proteins as well as growth factors/cytokines2,10,11
Keratinocyte stem cells are potent contributors to the Apligraf signaling profile
Research at Tufts Medical Center demonstrated that Apligraf contains keratinocyte stem cells.11 When compared to bilayered cellular construct generated without keratinocyte stem cells, their presence results in Apligraf generating8:
85%
more VEGF
62%
more IL-6
33%
more IL-8
The living cells of Apligraf
are bioactive and poised to heal9,12
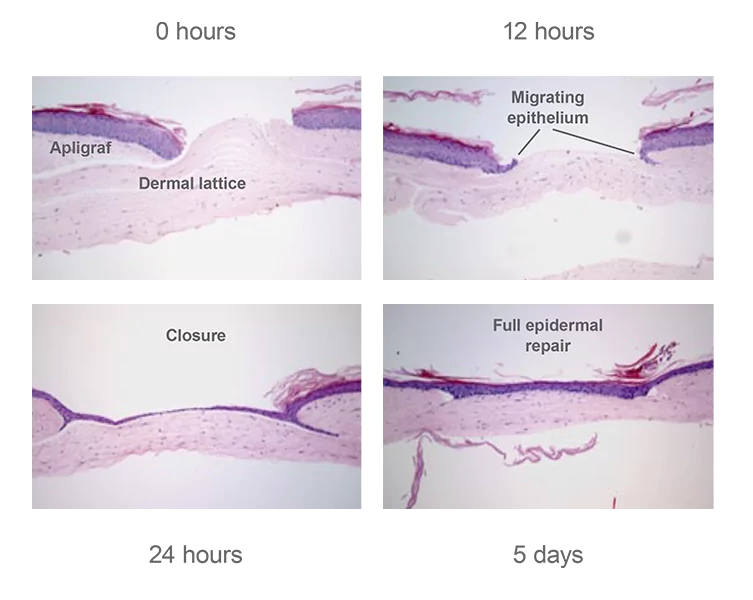
In an in vitro study, meshed Apligraf was incubated over a dermal lattice for up to 5 days. By 24 hours, the wound was closed—demonstrating that Apligraf had healed itself.9
Transforming wounds from chronic to acute
The living cells of Apligraf stimulate a potent healing mechanism, help restore normal healing functions, and put the wound back on track to heal1,9,12,13
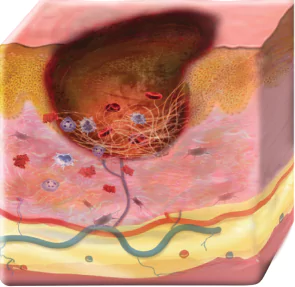
Before Apligraf treatment
- Keratinocytes and fibroblasts unresponsive/dysfunctional14-17
- ECM disorganized and MMPs imbalanced16,18,19
- Growth factor signaling dysfunction20,21
- Fibrosis present22,23
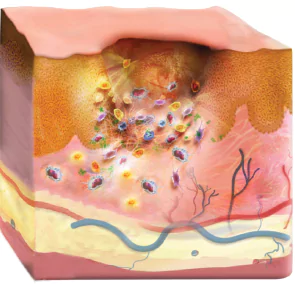
After Apligraf treatment
- Activated keratinocytes at the wound edge1
- Restored fibroblast function at the wound base, thus normalizing ECM production and MMP balance24
- Corrected and regulated growth factor signaling1,9,13
- Downregulated fibrosis formation24
Using Apligraf to help your VLU and DFU patients
See how to apply Apligraf, download a product factsheet, or contact an Organogenesis Tissue Regeneration Specialist today to get more information about how Apligraf transforms stalled wounds.
Contact usPlease refer to the Apligraf Package Insert for complete prescribing information.
REFERENCES:
- Stone RC, et al. Sci Transl Med. 2017;9(371). doi:10.1126/scitranslmed.aaf8611
- Apligraf [package insert]. Canton, MA: Organogenesis Inc; 2017.
- Marston WA, et al. Wound Repair Regen. 2014;22(3):334-340.
- Treadwell T, et al. Adv Wound Care. 2018;7(3):69-76.
- Sabolinski ML, et al. J Comp Eff Res. 2018;7(8):797-805.
- Veves A, et al. Diabetes Care. 2001;24(2):290-295.
- Kirsner RS, et al. Wound Repair Regen. 2015;23(5):737-744.
- Data on file. Organogenesis Inc.
- Milstone LM, et al. Wounds. 2000;12(5 suppl A):12A-19A.
- Schmid P. Wounds. 2000;12(5 suppl A):4A-11A.
- Carlson M, et al. Tissue Eng Part A. 2011;17(3-4):487-493.
- Falanga V, et al. J Invest Dermatol. 2002;119(3):653-660.
- Brem H, et al. Surg Technol Int. 2003;11:23-31.
- Mendez MV, et al. J Vasc Surg. 1998;28(5):876-883.
- Wall IB, et al. J Invest Dermatol. 2008;128(10):2526-2540.
- Cook H, et al. J Invest Dermatol. 2000;115(2):225-233.
- Hunt TK, et al. Adv Skin Wound Care. 2000;13(2 suppl):6-11.
- Kim BC, et al. J Cell Physiol. 2003;195(3):331-336.
- O'Donnell TF Jr, et al. J Vasc Surg. 2014;60(2 suppl):3S-59S.
- Barrientos S, et al. Wound Repair Regen. 2008;16(5):585-601.
- Vande Berg JS, et al. Surg Clin North Am. 2003;83(3):509-520.
- Smith PC. Int J Low Extrem Wounds. 2006;5(3):160-168.
- Werner S, et al. J Invest Dermatol. 2007;127(5):998-1008.
- Stone RC, et al. Wound Repair Regen. 2019. doi:10.1111/wrr.12778